Bone Graft
Bone Graft Beirut Lebanon for dental and oral surgery treatments
Bone grafting
Bone Grafting is a surgical procedure that replaces missing bone with material from the patient's own body, an artificial, synthetic, or natural substitute.
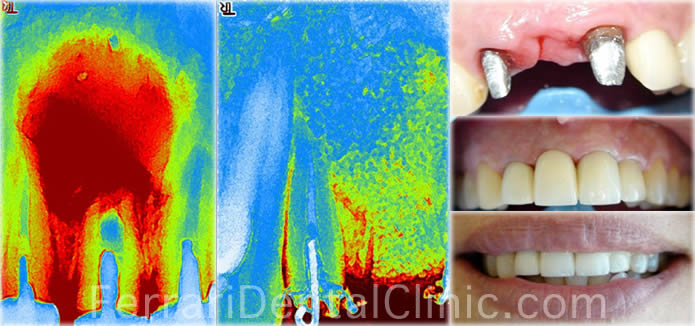
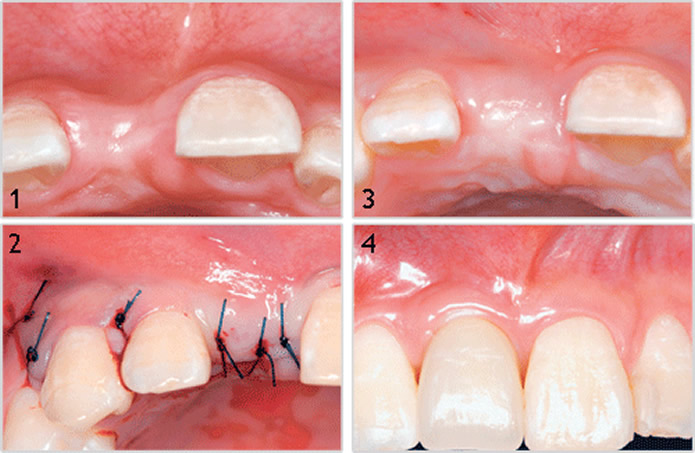
Maxillary Incisors: Massive dental cyst management - Bone Graft and prosthetic restoration: Before and After
 At Ferrari Dental Clinic we targeted on autograft, xenograft and especially Easy Graft cristal synthetic
At Ferrari Dental Clinic we targeted on autograft, xenograft and especially Easy Graft cristal synthetic
bone substitute from "Degradable solution" Switzerland.
Easy- Graft Principles:
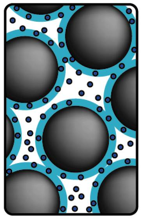
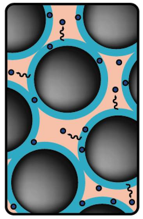
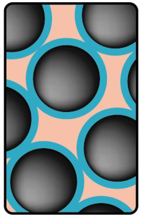
easy-graft™ products are bioresorbable, completely synthetic bone graft substitutes for bone defects. They consist of two components: Granules and BioLinker™. When combining these two components, the easy-graft™ material becomes a putty-like biomaterial and can be applied directly from the syringe into the bone defect. In contact with body fluids such as blood or saliva the material hardens within minutes and forms a stable, porous bone substitute material. Due to the porosity of the material, the absorption of blood is possible and thus positively influences the healing process.
 |
 |
 |
 |
| 1. Bio Linker + Coated BCP granules |
2. Adhesive granules: modeling in situ |
3. In situ Extraction of |
4. Formation of a porous solid body |
Fields of Application
easy-graft™ products are suitable for filling bone defects of the skeleton. The implantation site should be free of inflammation as well as soft tissue or granulation tissue. With our easy-graft™ products you can cover a wide range of indications in oral, orthodontic and facial surgery including:
- Augmentation of alveolar crest, possibly in combination with autologous bone and membranes (Guided Bone Regeneration, GBR)
- Filling of defect after Apicoectomy
- Filling of defects after removal of autologous bone
- Filling of defect after removal of bone cysts
- Sinus floor elevations
- Extraction defects in combination with membranes
- Filling of defects after surgical removal of retained teeth
- Periodontal defects in combination with membranes
Biological mechanisms governing bone grafting
|
Properties of various types of bone graft sources. |
|||
|
Osteoconductive |
Osteoinductive |
Osteogenic |
|
|
Alloplast |
+ |
– |
– |
|
Xenograph |
+ |
– |
– |
|
Allograph |
+ |
+/– |
– |
|
Autograph |
+ |
+ |
+ |
Bone grafting is possible because bone tissue, unlike most other tissues, has the ability to regenerate completely if provided the space into which to grow. As native bone grows, it will generally replace the graft material completely, resulting in a fully integrated region of new bone. The biologic mechanisms that provide a rationale for bone grafting are osteoconduction, osteoinduction and osteogenesis.The chart at right reveals which of these properties apply to the different types of bone graft material.
Osteoconduction
Osteoconduction occurs when the bone graft material serves as a scaffold for new bone growth that is perpetuated by the native bone. Osteoblasts from the margin of the defect that is being grafted utilize the bone graft material as a framework upon which to spread and generate new bone. In the very least, a bone graft material should be osteoconductive.
Osteoinduction
Osteoinduction involves the stimulation of osteoprogenitor cells to differentiate into osteoblasts that then begin new bone formation. The most widely studied type of osteoinductive cell mediators are bone morphogenetic proteins (BMPs). A bone graft material that is osteoconductive and osteoinduction will not only serve as a scaffold for currently existing osteoblasts but will also trigger the formation of new osteoblasts, theoretically promoting faster integration of the graft.
Osteogenesis
Osteogenesis occurs when vital osteoblasts originating from the bone graft material contribute to new bone growth along with bone growth generated via the other two mechanisms.
Types and Tissue Sources
Autograft
Autologous (or autogenous) bone grafting involves utilizing bone obtained from the same individual receiving the graft. Bone can be harvested from non-essential bones, such as from the iliac crest, or more commonly in oral surgery, from the mandibular symphysis (chin area) or anterior mandibular ramus (the coronoid process); this is particularly true for block grafts, in which a small block of bone is placed whole in the area being grafted. When a block graft will be performed, autogenous bone is the most preferred because there is less risk of the graft rejection because the graft originated from the patient's own body. As indicated in the chart above, such a graft would be osteoinductive and osteogenic, as well as osteoconductive. A negative aspect of autologous grafts is that an additional surgical site is required, in effect adding another potential location for post-operative pain and complications.
Autologous bone is typically harvested from intra-oral sources as the chin or extra-oral sources as the iliac crest, the fibula, the ribs, the mandible and even parts of the skull.
All bone requires a blood supply in the transplanted site. Depending on where the transplant site is and the size of the graft, an additional blood supply may be required. For these types of grafts, extraction of the part of the periosteum and accompanying blood vesels along with donor bone is required. This kind of graft is known as a free flap graft.
Allografts
Allograft bone, like autogenous bone, is derived from humans; the difference is that allograft is harvested from an individual other than the one receiving the graft. Allograft bone in taken from cadavers that have donated their bone so that it can be used for living people who are in need of it; it is typically sourced from a bone bank.
There are three types of bone allograft available:
Fresh or fresh-frozen bone
Freeze-dried bone allograft (FDBA)
Demineralized freeze-dried bone allograft (DFDBA)
Synthetic variants
Artificial bone can be created from ceramics such as calcium phosphates (e.g. hydroxyapatite and tricalcium phosphate), Bioglass and calcium sulphate; all of which are biologically active to different degrees depending on solubility in the physiological environment (see: Hench 'Bioceramics: From Concept to Clinic' 1991, Journal of the American Ceramic Society). These materials can be doped with growth factors, ions such as strontium or mixed with bone marrow aspirate to increase biological activity. Some authors believe this method is inferior to autogenous bone grafting however infection and rejection of the graft is much less of a risk, the mechanical properties such as Young's modulus are comparable to bone. The presence of elements such as strontium can result in higher bone mineral density and enhanced osteoblast proliferation in vivo.
Xenografts
Xenograft bone substitute has its origin from a species other than human, such as bovine. Xenografts are usually only distributed as a calcified matrix.
Alloplastic grafts
Alloplastic grafts may be made from hydroxylapatite, a naturally occurring mineral that is also the main mineral component of bone. They may be made from bioactive glass. Hydroxylapetite is a Synthetic Bone Graft, which is the most used now among other synthetic due to its osteoconduction, hardness and acceptability by bone. Some synthetic bone grafts are made of calcium carbonate, which start to decrease in usage because it is completely resorbable in short time which make the bone easy to break again. Finally used is the tricalcium phosphate which now used in combination with hydroxylapatite thus give both effect osteoconduction and resorbability.
Growth Factors
Growth Factor enhanced grafts are produced using recombinant DNA technology. They consist of either Human Growth Factors or Morphogens (Bone Morphogenic Proteins in conjunction with a carrier medium, such as collagen)