Orthodontic Surgery
 Not only is Cosmetic Tourism a widely recognized and appreciated concept today, it is actually taking off. The Hazmieh International Medical Center – HIMC established itself as a leader in the field of Cosmetic Surgery as well as non surgical procedures.
Not only is Cosmetic Tourism a widely recognized and appreciated concept today, it is actually taking off. The Hazmieh International Medical Center – HIMC established itself as a leader in the field of Cosmetic Surgery as well as non surgical procedures.
To accomplish the mission of providing the highest quality patient care, HIMC is distinguished by the outstanding training and backgrounds of our surgeons. HIMC team of doctors has more than 30 years of combined experience performing facial, skin, and body cosmetic surgery. They offer leading edge cosmetic procedures and have developed a number of innovative surgical techniques offered at few other facilities in the Middle East and in the world.
With visiting doctors from around the globe, the HIMC medical team strives to offer the most up to date range of services available today and insists to provide the highest standards of treatment that the medical profession can offer.
HIMC Services include Plastic surgery, Reconstructive surgery, Cosmetic Dermatology, The Esthetic Center, and The Laser, Esthetic and Surgical Dental Clinics.
Orthognathic Surgery
 Our orthognatic surgeries are performed at Hazmieh International Medical Center- HIMC- which includes an outstanding team of doctors and plastic surgeons...
Our orthognatic surgeries are performed at Hazmieh International Medical Center- HIMC- which includes an outstanding team of doctors and plastic surgeons...
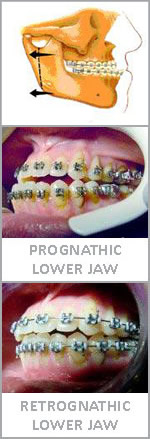
Orthognathic surgery is the type surgery performed by Oral Surgeons to correct skeletal mismatches. The word Orthognathic is derived from "ortho" meaning correct or straight and "gnathos" meaning jaw. These situations involve a situation where one of the jaws is:
- Too large
- Too small
- Too far forward or
- Too far back in relation to the rest of the skull.
Orthognathic Surgery is not intended to replace orthodontics for straightening the teeth when the relationship to the jaws is within the normal range, but cannot change the relationship of the jaw.
Orthognathic surgery is usually done in conjunction with orthodontics to provide the best possible end result.
Situations that lend themselves to Orthognathia are:
1. Apertognathia:
Is a situation when the back teeth meet but the front teeth do not touch. This space causes difficulty in biting with the front teeth.
2. Prognathia:
Is a situation where the lower jaw is too large and grows too far forward. Surgery can be used to slide the lower jaw back.
3. Retrognathia:
Is a situation where there is a "severe" overbite. These situations are managed with surgery and orthodontics together.
4. Vertical Maxillary Excess:
Also known as the gummy smile. In this case the upper jaw has grown too far down. Surgery can move the jaw upward to create a much nicer looking smile. If you believe you have any of these situations discuss them with your dentist who will refer to specialists qualified to carry out these procedures.
Orthognathic surgery is surgery to correct conditions of the jaw and face related to structure, growth, sleep apnea, TMJ disorders or to correct orthodontic problems that cannot be easily treated with braces. Originally coined by Dr. Harold Hargis, D.M.D., it is also used in treatment of congenital conditions like cleft palate .Bones can be cut and re-aligned, held in place with either screws or plates and screws.
Orthognathic surgery is performed by an oral and maxillofacial surgeon almost always in collaboration with orthodontic treatment, often including braces before and after surgery, and retainers after the final removal of braces. Orthognathic surgery is often needed after reconstruction of cleft palate or other major craniofacial anomalies. Careful coordination between the surgeon and orthodontist is essential to ensure that the teeth will fit correctly after the surgery. This coordination often necessitates that the surgeon be trained in dentistry, where complex concepts of occlusion between upper and lower teeth are taught. Unlike Oral and Maxillofacial Surgeons who are trained in dentistry, Plastic Surgeons receive no or minimal training. Thus, it is rare that an Orthodontist would find it appropriate for the surgery to be referred to a non-Oral and Maxillofacial Surgeon.
Planning
Planning for the surgery usually involves input from a multidisciplinary team. Involved professionals are Oral and Maxillofacial surgeons, Orthodontists, and sometimes a Speech and language therapist. As the surgery usually results in a noticeable change in the patient's face a psychological assessment is occasionally required to assess patient's need for surgery and its predicted effect on the patient.
Radiographs and photographs are taken to help in the planning and there is software to predict the shape of the patient's face after surgery, which is useful both for planning and for explaining the surgery to the patient and the patient's family. Advanced software can allow the patient to see the predicted results of the surgery.
The main goals of orthognathic surgery are to achieve a correct bite, an aesthetic face and an enlarged airway. While correcting the bite is important, if the face is not considered the resulting bony changes might lead to an unaesthetic result. Orthognathic surgery is also available as a very successful treatment (90-100%) for obstructive sleep apnea. Great care needs to be taken during the planning phase to maximize airway patency.
Procedure
The surgery might involve one jaw or the two jaws during the same procedure. The modification is done by making cuts in the bones of the mandible and / or maxilla and repositioning the cut pieces in the desired alignment. Usually surgery is performed under general anaesthetic and using nasal tube for intubation rather than the more commonly used oral tube; this is to allow wiring the teeth together during surgery. The surgery often does not involve cutting the skin, and instead, the surgeon is often able to go through the inside of the mouth.
Cutting the bone is called osteotomy and in case of performing the surgery on the two jaws at the same time it is called a bi-maxillary osteotomy (two jaws bone cutting) or a maxillomandibular advancement. The bone cutting is traditionally done using special electrical saws and burs, and manual chisels. Recently a machine that can make the bone cuts using ultra-sound waves has been introduced; this is yet to be used on a wide scale. The maxilla can be adjusted using a "Lefort I" level osteotomy (most common). Sometimes the midface can be mobilized as well by using a Lefort II, or Lefort III osteotomy. These techniques are utilized extensively for children suffering from certain craniofacial abnormalities such as Crouzon syndrome.
The jaws will be wired together (inter-maxillary fixation) using stainless steel wires during the surgery to insure the correct re-positioning of the bones. This in most cases is released before the patient wakes up. If the surgeon is not satisfied with the anchoring, he may elect to keep the jaws wired together. This is a considerably recent modification as the usage of the modern types of bone plates reduced the need for wiring the jaws together for a few weeks after surgery as was the case before. Some surgeons prefer to wire the jaws shut anyway to ensure proper healing of the bones, but they are becoming more of a minority among orthognathic surgeons.
Post operation
After orthognathic surgery, patients are often required to adhere to an all-liquid diet. After time, soft food can be introduced, and then hard food. Diet is very important after the surgery, to accelerate the healing process. Weight loss due to lack of appetite and the liquid diet is common, but should be avoided if possible. Normal recovery time can range from a few weeks for minor surgery, to up to a year for more complicated surgery.
For some surgeries, pain may be minimal due to minor nerve damage and lack of feeling. Doctors will prescribe pain medication and prophylactic antibiotics to the patient. Many doctors recommend that the patient rent a specialized machine that circulates cold water through pads on the face to help the swelling go down. Most of the swelling will disappear in the first few weeks, but some may remain for a few months.
The surgeon will see the patient for check-ups frequently, to check on the healing, check for infection, and to make sure nothing has moved. The frequency of visits will decrease over time. If the surgeon is unsatisfied with the way the bone is mending, he may recommend additional surgery to rectify whatever may have shifted. It is very important to avoid any chewing until the surgeon is satisfied with the healing.